The Brain Defense: Vets with head trauma, stress find mercy in court

Brock Hunter and Kris Parson. Photo Illustration by Steve Ravenscraft.
Not long after Kris Parson returned home from the war in Iraq, his girlfriend began calling the police to their house in Coon Rapids, Minnesota, a suburb about 15 miles north of Minneapolis. She’d dial 911 to report that she and Parson were fighting, and that she was afraid he was going to hurt her. Every time police came to the house—on at least a dozen occasions—things would calm down and the officers would leave.
The police found no evidence that Parson, who served as a combat engineer with the Minnesota National Guard, had physically hurt his girlfriend, and he hadn’t done anything to warrant an arrest.
Then one night she called the police again. This time she said Parson had put his hands around her throat and tried to strangle her. The police arrested him on felony charges of domestic violence.
While he was being booked at the jail, Parson knew just whom to call. There was this lawyer over in Minneapolis who handled lots of cases for veterans and had once represented him on a drunk driving charge. The guy understood veterans and how the war had messed them up. He knew what was going on in their brains and could help. His name was Brock Hunter.
Hunter has developed a specialty in representing veterans charged with crimes outside the military justice system. He and his colleagues in this area offer a version of the brain defense, an approach that considers the possible influence of post-traumatic stress disorder, depression and traumatic brain injury caused by their military experience on their clients’ criminal behavior. They seek understanding and treatment instead of prison and, in some cases, mercy instead of execution.
Lawyer-Veteran
Hunter is a veteran himself, having served four years in the Army, mostly as a sniper scout in the tension-filled demilitarized zone of Korea during the late 1980s.
When he returned, he spent a few years in college not knowing what he wanted to do, went to law school and joined a corporate firm. He hated it. Big button-down firms were a terrible fit for a freewheeling, spirited man with a passion for social justice.
After leaving that job, Hunter took on criminal cases and worked for the local public defender’s office. He soon began to see lots of veterans pulled into the criminal justice system, including Vietnam vets. Many were homeless and addicted to drugs and alcohol and seemed deeply wounded psychologically. In the years following the 9/11 terrorist attacks, he saw veterans in court who had come home from the wars in Afghanistan and Iraq, and his attachment to them grew stronger.
On a kayaking trip around Lake Superior’s Apostle Islands in 1999, Hunter stopped at the nearby town of Ashland, Wisconsin, and browsed in a used-book store. There he happened to see a copy of Achilles in Vietnam: Combat Trauma and the Undoing of Character. The book by Dr. Jonathan Shay, a psychiatrist, draws comparisons between the experiences of modern combat veterans and those in Homer’s Iliad and Odyssey.
The warriors 3,000 years ago, Shay observes, suffered the same kinds of psychological wounds as their modern counterparts. In the Iliad, Achilles experiences profound grief after losing a friend in battle, goes berserk and mutilates enemies. In the Odyssey, after the Trojan War, Odysseus and his men pillage a city and get addicted to drugs. When he finally comes home, Odysseus slaughters men who had been courting his wife while he was at war. He lost his mind.
Something in Hunter clicked while he was reading Shay’s book, and he couldn’t stop turning the pages as he stood in the bookstore. “It changed everything,” Hunter says. “That was a turning point for me.”
Hunter decided that he had found a special niche and a mission as a lawyer. He immersed himself in research and literature about veterans, looking closely at how PTSD and traumatic brain injuries affect them. He decided to dedicate his practice to helping veterans navigate the criminal justice system and receive treatment rather than prison time. He believes his fellow citizens should place high value on the nation’s military personnel for their service—regardless of the politics of war—and be willing to give them a few breaks because of their sacrifices for the country.
A Harrowing Battle
Kris Parson can be an intimidating figure. Muscular and lean, he stands about 6 feet tall with a square jaw and intense brown eyes. His voice is deep, probably thickened by the cigarettes he chain-smokes. His speech is hesitant at times, as if his words are a few beats behind his thoughts. He was diagnosed with a TBI after surviving a harrowing attack by insurgents against U.S. and Iraqi government troops in Sadr City.
I’m talking to Parson in his home in Coon Rapids, the shades drawn and most of the lights off. During the attack, he was hunkered down in a concrete building.
“I remember nine blasts. I felt this huge wave. I didn’t hear anything—you just feel it. Things started coming through the wall. I didn’t know if I was alive or dead. I had an out-of-body experience.” His head felt as if someone were stomping on it or striking it with a bowling ball. Then came a feeling of euphoria. “Is this real?” he wondered.
The blasts stopped. “I remember getting up and saying, ‘Awesome, man!’ Cause that’s what you do,” he tells me. “Life got really weird after that.”
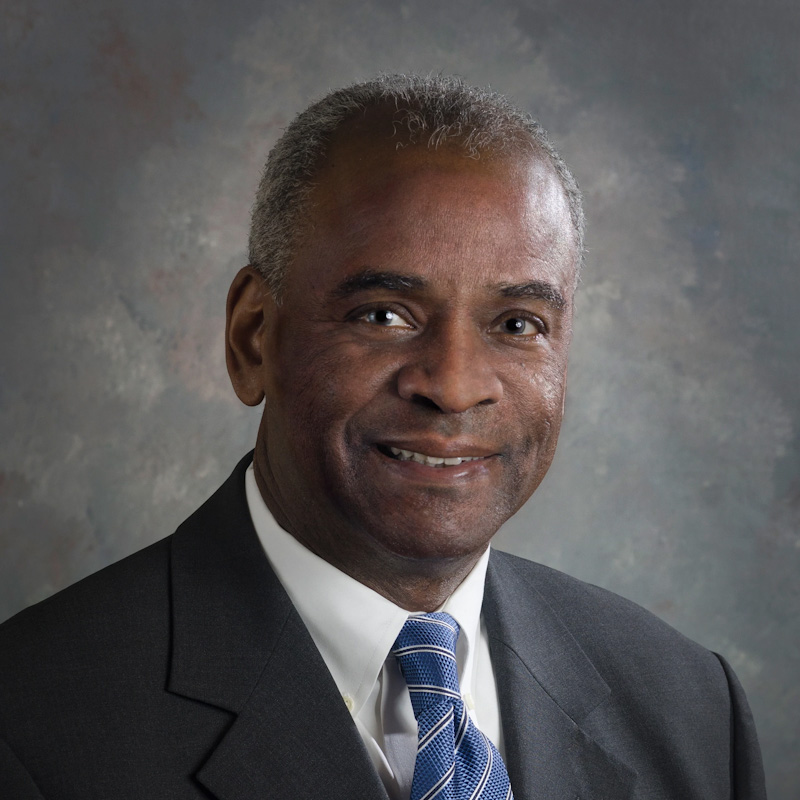
The Brain Defense, released on Feb. 28, is the latest nonfiction book about the criminal justice system by Kevin Davis, an assistant managing editor at the ABA Journal.
Blast injuries like those Parson suffered are signature wounds of the wars in Iraq and Afghanistan, primarily because of the prevalence of improvised explosive devices. According to one estimate, more than 50 percent of injuries sustained during those conflicts were the result of explosives. That includes bombs, grenades, land mines, mortar and artillery shells and IEDs. The most common cause of injury among American soldiers at Walter Reed National Military Medical Center is blast injuries, accord-ing to the Defense and Veterans Brain Injury Center. By 2008, as many as 400,000 troops in Afghanistan and Iraq had experienced mild to severe TBIs. Many were never diagnosed.
Multiple blast injuries can feel like being hit by a wave and then being pulled back into the surf. The explosion triggers an intense rise in atmospheric pressure, which has the force to push organs within the body and then release them when the pressure falls again.
Parson may seem to have emerged physically unscathed because he had no penetrating head wounds or blunt trauma to the outside of his skull. But a sudden jerk of the head, along with the blast pressure, can cause shearing within the brain, tearing arteries, veins, connective tissue and nerve fibers. It gets even more complicated inside the brain’s gray and white matter: Its variations in weight, density and structure cause it to move at different speeds than the blast, damaging the dense layers of neurons throughout the cerebral cortex. The long, microscopic axons—the conduits that communicate information throughout the brain—are stretched, pulled and twisted, resulting in what’s called a diffuse axonal injury.
A heavy blast can result in more damage to a brain than a penetrating wound from a bullet or shrapnel. Multiple blast injuries like Parson’s, in which his head went back and forth and shook from side to side, can compound the damage and cause a variety of physical, emotional, cognitive and behavioral symptoms. And many of these symptoms emerge with other conditions such as depression or PTSD.
Microscopic damage at the neuron level, often caused by traumatic brain injury, is not always as evident as a penetrating brain injury might be, and among combat veterans in Iraq and Afghanistan it became known as the invisible injury. The effects of TBI suggest its presence. Studies have shown that people with traumatic injury have greater impulsivity and a greater propensity to aberrant behavior. Soldiers with TBI often sense that something is not quite right but can’t figure out what or why. Their relationships suffer, they lose concentration, or they become distracted on the job. The incidence of substance abuse is high among those with TBI.
That’s exactly what happened to Parson.
It’s not clear how TBI and PTSD intertwine, or whether those who suffer from one or both are more likely to commit crimes and acts of extreme violence than others. Many veterans who suffered through combat and are afflicted with TBI and PTSD have never committed crimes or hurt others. They feel hurt and resentful when people assume they’re capable of violence or homicidal rage. The stigma may even prevent them from seeking treatment, and those who suffer from PTSD are more likely to harm themselves.
More Court Options
In 2007, Hunter helped draft a Minnesota law that permits judges to consider the option of sending veterans to treatment programs if they suffer from combat-related mental health disorders. The law requires courts to ask whether a criminal defendant is a veteran and allows their lawyers to order psychological evaluations. If a defendant is diagnosed with a mental health disorder, the court can work with the Department of Veterans Affairs on a treatment plan as part of the sentencing.
About a year after Hunter helped create the Minnesota law, a special veterans treatment court was established in New York. Robert Russell, an associate judge for the city court of Buffalo, had noticed more veterans showing up in his drug and mental health treatment courts. His idea was to create a court especially for veterans. Since then, more than 220 such courts have been established across the country to take into account that those who return from war often turn to drugs or alcohol to alleviate suffering from physical, mental and emotional damage.

Kevin Davis
These courts help veterans receive the government-provided services they are entitled to, but may not be aware of or have ignored. Veterans who stay clean and out of trouble can have their criminal charges dismissed and records wiped clean.
In 2009, Hunter won a landmark case that resulted in the kind of collaboration he’d sought to get veterans help instead of prison. His client, Arthur Torgesen, was a Vietnam vet who suffered from severe PTSD and had a history of depression and alcoholism. He was charged with second-degree murder and arson for stabbing his wife, Sherrill Harnden, and setting their home on fire. By common legal standards, he would not qualify as insane because he was aware of his actions at the time of the crime and understood that what he did was wrong.
His confession suggested he had carefully thought through his plan. He was stressed about a recent cancer diagnosis and financial trouble and had decided to kill himself. Even though he’d been with his wife for 25 years, they’d been married for just a year. Torgesen said in his confession that he was afraid she wouldn’t receive his military benefits after he died. Rather than let her suffer and go broke, he decided to take her life and then his own. After he stabbed her, he drank wine, called relatives to say goodbye, doused himself with gasoline, and set the house on fire. He fled the burning home but was badly injured.
Hunter suggested to the judge that Torgesen receive mental health treatment rather than prison time. At Hunter’s request, the Anoka County prosecutor, Bob Johnson, consulted with Harnden’s family about a plea agreement that would allow Torgesen to go directly to a mental health facility. The family felt it was the right thing to do.
Hunter started getting national press attention for his work; the New York Times quoted him in a series about veterans charged with murder. Demand for his services grew. In hometowns across the country, veterans were getting arrested for domestic violence, drunk driving, fights and other crimes.
High-profile cases drew even more attention. In Fort Carson, Colorado, returning soldiers were arrested for fighting, beatings, rapes, DUIs, drug deals, domestic violence, shootings, stabbings, kidnapping and murder. The violence prompted the Army to commission a study called the epidemiologic consultation to examine why veteran violence was increasing. It found that the murder rate at the base had doubled, and the number of rape arrests tripled. From 2005 to 2008, 13 soldiers at Fort Carson were charged with homicide.
Soldiers from one particular unit, known as the Lethal Warriors, were charged with most of the murders. Members of that unit, which by reputation had served in the most violent battlefields in Iraq, also had a rate of PTSD three times that of other units.
The report found “a possible association between increasing levels of combat exposure and risk for negative behavioral outcomes.” However, it also cited other risk factors, such as criminal histories and experiences of drug and alcohol abuse. The report was careful to note that “overall, most soldiers are doing well.” Many, it pointed out, had seen heavy combat and had risk factors for violence yet committed no crimes.
Then in 2012, Army Staff Sgt. Robert Bales was charged with killing 16 unarmed Afghan civilians inside their homes—the worst civilian murder spree ever by a single solider. Bales had sneaked out of his base in southern Afghanistan and into a walled compound, where he inexplicably beat and kicked a group of civilians, shot them, and set several bodies on fire.
His lawyer suggested Bales was a good soldier who had had a mental breakdown due to PTSD and a TBI that he had suffered during his four deployments. Bales eventually pleaded guilty. At his sentencing hearing, he tearfully apologized to the families of his victims but gave no explanation. He did say that after returning from tours in Iraq, he felt angry, weak and fearful, and quit counseling because he saw no improvement. His prosecutors characterized him as a frustrated man with financial and marital problems, prone to drinking and violent outbursts.
Lost at Home
In the weeks and months after Kris Parson survived the blast attacks in Iraq, he came to realize that he was damaged in ways he hadn’t expected. His scratches and cuts had healed, but he felt strange. “I couldn’t speak a whole sentence after that,” he says. “People would say to me: ‘Are you drunk?’ “
When Parson finally came home to Minnesota, he had trouble making the transition to civilian life. He was unable to find work and felt lost. His difficulty in speaking was a liability in job interviews. He suspected his wife was having an affair, and their marriage ended soon afterward. He started drinking every day. He had haunted dreams, reliving some of the attacks, the explosions and the sounds of people getting wounded. “There was a lot of screaming,” he recalls. “One of the worst things to hear is another man screaming.”
Parson spent many of his days at the VA for speech therapy and treatment, and the rest of the time drinking. “For four or five years, I didn’t feel like I was alive,” he says. “I still feel like that sometimes. A lot of things don’t make sense to me anymore.”
He loved to read but couldn’t remember what he read or would remember only much later. He felt volatile but did not realize the extent of his simmering anger. “You don’t really understand until you scare the living shit out of someone,” he says. “Everything bothered me. Everything made me mad. I was pumped with adrenaline.”
That first year home was the worst. “I was really needy,” he says.
“I drank every single day. I planned to hang myself.”
One night Parson did try to kill himself, but not by hanging. He crushed a handful of sleeping pills and mixed the powder with beer to make it go down easier and absorb faster. Then he drank four beers. He must have passed out. He heard pounding on his front door, and then someone kicked in the door. It burst open, and men in black stormed in. Parson’s military mind and combat experience took over—people in the dark were the ones who attacked him in Iraq. He went wild, swinging and hitting cops—he hurled one cop into a wall. They finally subdued him. In an act of mercy, rather than arrest him they took him to a VA mental health facility. He’s not sure who called the cops that night, but that person saved his life.
Parson was not himself in those days. “I can get violent,” he recalls. “But it’s not on purpose. It’s my natural reaction. I’m surprised they didn’t shoot me.” He used to sleep with a knife but for some reason did not that night. “Thank God I didn’t.”
TBI and Violence
Parson first encountered Hunter by accident. He’d been arrested for drunk driving and had searched the internet for a local attorney. Hunter seemed like a good candidate, though Parson didn’t know that he was a veteran. When they spoke on the phone for the first time, Hunter intuitively asked whether Parson was in the military. Parson told him about his experience.
“You were in Sadr City?” Hunter asked. Then he knew Parson likely had some post-combat problems.

400,000 troops in Iraq and Afghanistan experienced traumatic brain injuries, many undiagnosed, according to estimates from 2008.
Parson is typical of the veterans Hunter represents. High-profile murder cases receive national and international attention, but most veterans charged with crimes are not accused of murder. More likely they’re arrested for domestic violence, fighting, drugs or drinking. Many have TBI, and their anger is easily triggered—even by someone they perceive is looking at them the wrong way. Drinking is the favored way to self-medicate, as it was for Parson, whose girlfriend liked to drink, too, he says. After his marriage ended, Parson met his girlfriend at the gym, and soon afterward she moved into his house with her two kids. She was unemployed. They spent a lot of time drinking together.
“It was a combination of things,” Parson says. “It was a matter of time before it would blow up.”
In 2011, Hunter got a phone call from Floyd “Shad” Meshad, a nationally known, highly regarded veterans’ advocate. Meshad had been a medical service officer during the Vietnam War and founded the National Veterans Foundation. He was a leader in recognizing and treating soldiers with PTSD. In the late 1980s, Meshad’s foundation published Defending the Vietnam Combat Veteran, a guide for attorneys representing veterans in criminal court. Now, in 2011 Meshad had a proposition for Hunter: Would he be willing to help put together an updated version of his book to assist lawyers defending the more recently returned veterans? “He heard about the stuff I was doing and invited me in,” Hunter says. “It was like getting a call from Elvis. He is an absolute hero.”
Hunter did help assemble, write and edit The Attorney’s Guide to Defending Veterans in Criminal Court. With chapters written by experts from the fields of law, medicine, social work, psychology and psychiatry, the book offers practical advice on defending veterans with PTSD, TBI, substance abuse and other service-related disorders.
Favored Treatment
Parson got special treatment because he served the country. After his arrest, Hunter was able to get his domestic violence case transferred to the special veterans court in Anoka County. Hunter worked out a deal with the prosecutor: Parson would undergo therapy, check in with the court periodically, and stay out of trouble for 18 months. If he could do that, he would not have a felony conviction.
Was it fair that Parson received special treatment because he was a veteran? Veterans returning from Vietnam had to struggle to gain access to proper treatment for their physical and mental wounds. Those coming back from Iraq and Afghanistan have found a much different atmosphere. There’s a greater recognition of TBI and of the mental toll of combat, and an acknowledgment of PTSD as a legitimate diagnosis. Today’s veterans are in a better position than their predecessors to cite mental health issues and brain injuries as contributing factors to criminal behavior.
Thomas L. Hafemeister, a professor at the University of Virginia School of Law, has written extensively about PTSD, veterans and the criminal justice system.
“The veterans from Iraq and Afghanistan were generally viewed as a sympathetic population,” he told me. “They’ve done a great service for the country and through no fault of their own have gone through some horrific events. So it feels really wrong to throw the book at them. They don’t seem as deserving of the full strength of the law as other criminal defendants.”
But this line of reasoning poses constitutional problems, he points out: “Under our criminal justice system, we have fair and equal treatment under the law. So how do we defend carving out special rules for this population? Do we have one set of rules for a population seen as sympathetic and another for a population seen as unsympathetic? That goes against the notion that justice is blind.”
Brock Hunter has an answer: America’s justice system already has a decadeslong history of using special courts for drug offenders and those with mental health problems. “These courts are based not on the philosophy of sympathy but upon the recognition that treating offenders’ underlying issues, rather than just punishing their associated behaviors, dramatically reduces the likelihood of recidivism and enhances public safety,” he says. “Veterans courts operate on the same philosophy.”
The legal ground may already be shifting when it comes to handling veterans with brain injuries and PTSD. “The legal system has been hesitant about embracing the insanity defense,” Hafemeister says. “But the question that came with all these veterans coming back with PTSD and these other mental disorders was whether the criminal justice system would change its view about this type of defense.”
Moving On
Parson has a newly acquired skill in building computers, which he learned by trial and error and through online courses.
To him, it’s simple. “Can you add one plus one? That’s computers,” he says. He also studies marketing and business and takes free online computer courses from Microsoft and Cisco Systems. “I have to have a challenge in my head,” he says.
He’s extremely sensitive to light—especially sunlight. When he goes outside, he wears glasses that are nearly black. Inside his home, the curtains and shades are always drawn.
He still has nightmares. “I’ve had them so long that it’s normal,” he says. In these dreams, he is in a firefight and runs out of ammo. He destroys a building. He grinds his teeth at night so badly that he had to have five of them surgically removed and replaced.
“Even if I might look good, there’s always stuff going on inside,” he tells me.
I ask Parson if he is afraid he might lose control and hurt someone because of his brain injury. The TBI, he says, “really messed with me. ... I’ve learned how to manage it better.” But “if people cross my boundaries ... ” He pauses and stops, lost in thought. “People don’t understand what’s going on.”
Hunter’s not looking to excuse anyone’s behavior. “Injuries like TBI and having PTSD can drive behavior that gets [veterans] in the criminal justice system,” Hunter explains. “We’re not saying they need to escape responsibility. If they can get the help they need, let’s give it to them. If not for their service or experience with the military, they might not be involved in the criminal justice system.”
Parson feels fortunate to have found Hunter to help him through his legal and personal troubles. With the support of other stakeholders in the court and the local veterans community, Hunter helped him avoid foreclosure on his home.
“I believe Brock has a lot of passion,” he says. “He really connects the dots and puts all this stuff out there.
“It can look like I’m a terrible person, but I’m not.”
This article is an excerpt from the book The Brain Defense: Murder in Manhattan and the Dawn of Neuroscience in America’s Courtrooms by Kevin Davis, an assistant managing editor at the ABA Journal. It appeared in the March 2017 issue with this headline: “The Brain Defense: A better understanding of head trauma and stress helps vets in trouble find mercy.”