Personal injury lawyers turn to neuroscience to back claims of chronic pain

Illustration by Sam Ward
Blobs of 300-degree tar hit Koch, 36, on the right side of his face and ear, and adhered to his right arm, causing first- and second-degree burns. The pain was so severe that doctors had to give him several doses of morphine.
Koch’s burns eventually healed, but more than a year after the accident, he complained that he continued to feel pain in his right arm, which prevented him from working or helping around the house.
He sued his employer, Western Emulsions, for damages, claiming that the nerves beneath his right arm never fully healed, and that he suffered from chronic neuropathic pain. The company’s attorney alleged that Koch was faking.
Koch’s lawyer, Roger Strassburg, needed to prove that his client really was in pain. But that was going to be tough. There was no such thing as a pain meter to measure or confirm its existence. Pain is subjective, its sensations and intensity known only to the person experiencing it.
“I asked my clients’ chronic pain manager if there was any evidence I could use to show whether my client was in pain or not,” Strassburg says. “And he mentioned fMRI brain scanning.”
Functional magnetic resonance imaging is used to measure activity in the brain by detecting blood flow. When certain parts of the brain are active, blood flows to those regions and can be detected by the scanner through a complex process in which the scanner’s powerful magnet tracks blood oxygen levels. Researchers have been using fMRI to test theories that they could pinpoint locations in the brain that become active with pain.
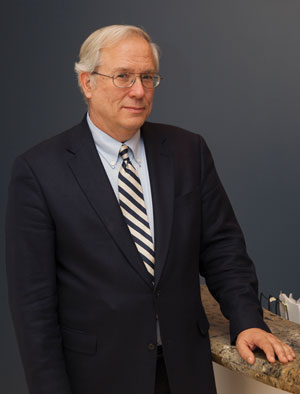
Roger Strassburg. Photograph by Bob Torrez.
While some early studies identified areas of the brain that became active when people experienced pain, the research was far from definitive. Still, Strassburg was willing to give fMRI a try. “I think I must have called every fMRI lab in the country,” he says.
The labs kept turning him down, until he reached Joy Hirsch, then a professor in the departments of neuroscience, radiology and psychology at Columbia University in New York City and director of its fMRI research center. One of Hirsch’s specialties was mapping the brain for neurosurgeons so they could avoid damaging essential functions during surgery.
Hirsch told Strassburg that she would scan Koch’s brain at no cost because she was interested in the case as a scientist. Strassburg arranged for his client to visit New York.
PUTTING A PRICE ON PAIN
Chronic pain is a national public health problem and an expensive one. It’s typically characterized as pain that’s persistent and lingering, as opposed to acute pain, which is sudden and sharp. Chronic pain often continues after injuries have healed, lasting for months or years, and can be debilitating. According to a 2011 report from the Institute of Medicine, about 100 million Americans suffer from chronic pain, costing society as much as $635 billion annually for everything from health care expenses to lost productivity at work. Pain is frequently cited as a factor in assessing damages in personal injury litigation and workers’ compensation cases, and can significantly boost the size of awards, depending on its severity.
That’s where things get tricky. Because there are no standardized or widely accepted diagnostic tools that can accurately or objectively measure pain, lawyers can easily challenge it. Patients are usually asked to rate their pain on a scale of 1 to 10 and sometimes are shown a poster of cartoon faces whose expressions indicate the severity of pain. The problem is that one person’s 5 might be another’s 10.
Some people do indeed exaggerate pain, which leads defense lawyers to be initially suspicious of claims for damages. It’s also the reason many physicians are cautious about how they treat pain, concerned that they might be complicit in creating or feeding addictions to painkillers for those who may not really need them.

Joy Hirsch. Photograph by David Fonda.
Because of the magnitude of chronic pain’s impact, researchers have been seeking ways to better identify, understand and treat it. Neuroscientists in particular have been working to identify patterns of brain activity associated with pain that might help lead to better targeted treatments.
But personal injury lawyers see another potential value to neuroscience—as a way to document their clients’ pain if and when it might be contested. The problem, many scientists say, is that the research, while showing much promise, is still in its nascent stage.
MEASURING PAIN
In May 2007, nearly two years after the tar accident, Koch met with neuroscience specialist Hirsch and prepared to have his brain scanned with an fMRI machine while performing simple motor tasks.
Hirsch took images during tests in which Koch squeezed a rubber ball using his right hand (the injured, painful side) and his left hand. The theory was that the images would show patterns of brain activity associated with pain when the right side was stimulated, but not the left.
Koch said that before the test, as he was resting, the pain he felt in his right arm rated between 3 and 4 on a scale of 1 to 10. But when he squeezed the ball, his pain rose to a 9.5. He reported feeling no pain in his left arm. From the images, Hirsch reported increased activity (blood flow) in the bilateral superior frontal gyrus, bilateral cingulate gyrus and the primary motor areas—all of which she described as “a component of a well-known pain-mediating neural circuit.”
Hirsch explained in her report that functional brain mapping is based on the fundamental principle that specific functions and sensations are mediated by specific regions of the brain—including visual, sensory and motor functions—and is routinely used prior to neurosurgery to protect those regions. Her readings on the scans, she said, were consistent with Koch’s rating of pain intensity when he squeezed the ball with his right hand.
Hirsch said the fMRI exam offered the perfect, built-in control to bolster Koch’s contention that his pain was not imagined. The movement of Koch’s right arm caused pain, which was indicated in activity of the brain scan, while the other did not trigger similar activity in that part of the brain.
Attorney Strassburg was ready to take his evidence to court.
BILLIONS AT STAKE
Around the time of the Koch case, law professor Adam Kolber was doing some of his own investigating into the use of neuroscience for documenting pain. He published a paper in the American Journal of Law & Medicine that offered a look at how neuroscience might be valuable in the courtroom—not right away, but someday. It raised the legal and ethical issues that would likely result from using the science in court.
Kolber, now at Brooklyn Law School, noted that pain is one of the easiest medical complaints to feign, which makes it a problem because pain and suffering awards represent about half of all personal injury damage awards. “Even if a small percentage of those awards involve feigned or grossly exaggerated symptoms, billions of dollars may be redistributed each year to malingering plaintiffs,” he wrote. “On the other hand, if litigants raise genuine claims that we fail to recognize, billions of dollars may fail to reach those who properly deserve compensation for injuries.”
Researchers have tested methods to document pain since at least the 1960s, according to Kolber. Some employed a process known as thermography, which used infrared radiation to measure surface body temperatures. The temperature was supposed to be an indicator of soft-tissue injuries or other painful conditions. But thermography had a high rate of false positives and mixed results in being admitted as evidence.
With the advent of positron emission tomography scanning in the 1980s and, more recently, fMRI scanning, researchers have been better able to record brain activity and have done a number of studies seeking to link the experience of pain to specific regions in the brain. The debate remains over whether that brain activity can be directly correlated to pain.
Kolber points out that while malingerers may fabricate their pain, it’s far more common for people who are in pain to modestly exaggerate its intensity in legal proceedings. Even plaintiffs who don’t exaggerate their symptoms may have difficulty expressing the nature of their pain. That’s where brain scanning may help those who need it.
DISPUTING THE FINDINGS
Attorneys for Western Emulsions were not willing to accept Hirsch’s claim that a brain scan could show Koch had chronic pain. They filed a motion seeking to keep her from testifying, describing the science behind her opinion as “highly questionable, speculative and unproven.” The motion also sought a Frye hearing before Judge Javier Chon-Lopez of the Arizona Superior Court in Pima County to determine whether Hirsch’s testimony would even be admissible under Arizona law. Under the Frye standard, Hirsch’s expert opinion would be admissible only if the technique was generally accepted as reliable in the relevant scientific community.
Western Emulsions hired a well-regarded pain researcher to challenge Hirsch’s claims. Dr. Sean Mackey, a pain expert and neurologist at Stanford University, said that the brain activity shown in Hirsch’s scans could have been triggered by any number of factors, including the possibility that Koch was simply thinking about pain.
Mackey also suggested that people can “cheat” the scan by imagining their pain was more severe than it was. He had conducted earlier experiments in which volunteers touching a hot plate while in a scanner were able to conjure more intense pain, and thus brain activity, when they watched a video of flames.
Hirsch countered in her deposition that cheating is not possible because re-creating sensation in the mind is all but impossible. She also said that she detected no signals indicating imagined pain.
The critical issue in the case, Mackey said, was the subjectivity of pain. “This is akin to using fMRI to detect the presence of love, hate, anxiety, anger or any other human emotion or cognition,” Mackey said in a deposition. “In essence, we are attempting to read someone’s mind with fMRI. We just cannot do that at this time.”
Judge Chon-Lopez denied the motion, stating that Hirsch’s testimony “will be based on a combination of generally accepted scientific principles (fMRI) and inductive reasoning from her own research and calculations involving patients with chronic pain, including plaintiff Koch.” The judge noted that a Frye hearing was inapplicable when a witness reaches a conclusion by inductive reasoning based on his or her own experience, observation or research. “In this case, the validity of Hirsch’s testimony can be tested by interrogating her.”
Hirsch never had to take the stand. A short time later, Western Emulsions agreed to settle the case for $800,000. The attorney who handled the case for the company did not respond to ABA Journal requests to discuss it.
NEUROSCIENTISTS IN DEMAND
News of the settlement circulated among personal injury lawyers, and Hirsch began to get requests to perform similar scans to document pain. “The judge sided with me on the substance and validity of the technique,” says Hirsch, now a professor at Yale University. “This was similar to, but not exactly the same as, what we do with neurosurgical planning.”
Hirsch says that by accident, she became known as a brain and pain imager. “It’s not something I really wanted to do,” she says. Since then, she has scanned dozens of people, though she’s rarely had to appear in court because most of the cases were settled.
One of the lawyers she’s worked with is Michael Flomenhaft of the Flomenhaft Law Firm in New York City, which bills itself as “a neuroscience-focused firm.” Flomenhaft began using neuroscientific evidence more than a decade ago while representing plaintiffs who had traumatic brain injuries from concussions.
Defense attorneys, he says, often disputed his clients’ head injury claims and invariably found physicians who would testify that they found no evidence of brain damage. “It was the invisible injury,” Flomenhaft says. “I couldn’t accept early in my career what was being pronounced to me by physicians.”
Flomenhaft began studying neurology, which led him to neuroscience and brain imaging. He met Hirsch when he taught a course in neurolaw at Columbia and began to learn about brain imaging for pain.

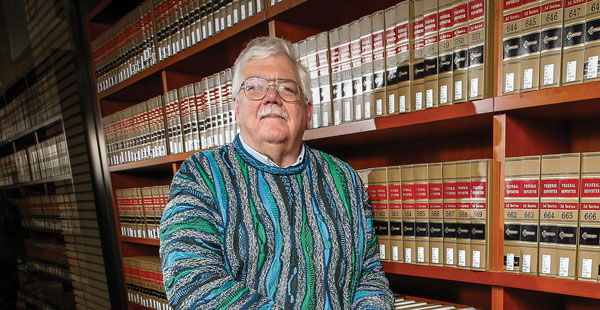
Michael Flomenhaft. Photograph by Arnie Adler.
He was particularly struck by the work of Northwestern University researcher Vania Apkarian, who also has used fMRI to document pain. In one of his studies, Apkarian scanned the brains of people shortly after their back injuries, and again later. Apkarian found they developed chronic back pain but, interestingly, the locations that signaled pain in their brains shifted from areas associated with acute pain to areas where the brain regulates emotions.
“He explained that chronic pain is a brain injury,” Flomenhaft says. “Case by case, I began to see the neuroscience implications of things.”
While fMRI has not been embraced by the scientific community as a comprehensive diagnostic tool to show the presence, or absence, of pain, Flomenhaft says it can show brain activation when a person is experiencing pain, which should be enough for the courts. “We are trying to show a jury what’s there, not make a diagnosis,” he says. “This is validating, objectively, that there is pain and the neuroscience has a really good foundation,” he adds.
Scientists, by nature, are cautious, Flomenhaft says. “The confidence level is different in the law,” he says. “When you’re dealing with elite scientists, you’re always dealing with their confidence level. Their language is always different. They use words like ‘may,’ ‘suggest,’ or ‘could.’ “
He believes brain scans are going to be seen more frequently in the courtroom. “The doors are opening, but they’re opening very slowly,” he says. “Neuroscience can recast all kinds of things about law. It’s revolutionary, and there’s all kinds of resistance to neuroscience. It’s for judges to decide what’s ready for the courtroom, not scientists. Judges decide what’s admissible.”
Hirsch also believes the science will and should have value in the legal setting. “Why after all this time are there no techniques to use this in a credible way to assist people who really, really need assistance in terms of the law, in terms of personal injury?” she asks. “Personal injury often has a bad reputation, but there are many people who really, really deserve compensation for injuries, like Mr. Koch.”
The doors are indeed opening, albeit slowly, and creating opportunities for private companies to offer brain scanning for lawyers. A Ridgefield, Connecticut-based company called Millennium Magnetic Technologies advertises, among other diagnostic services, brain scanning to validate the presence of pain.
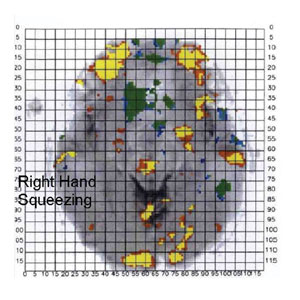
Functional magnetic resonance imaging. Carl Koch’s brain scan nearly two years after the accident shows that he experienced extreme pain when moving the injured side of his body, according to neuroscience specialist Joy Hirsch.
“We’re working with people who have pain and documenting that pain objectively for legal purposes,” says Dr. Steven Levy, the company’s CEO. “It can also be used to quantify the amount of pain, and this can be helpful in determining what is just compensation based on something objective.”
The procedure costs $4,850 and includes three scans required for the pain study. Levy says clients should consider it a smart investment to support their cases. The company uses fMRI scans taken before, during and after staff induce pain in the patient’s troubled areas. The scans are then analyzed through the company’s “Rosetta technology,” which it says “involves specialized imaging algorithms, customized sensory input, computational neuroimaging processes, and utilizes pre-certified imaging centers.”
The Rosetta process was created by Dr. Donald H. Marks, MMT’s chief science officer and founder. While Marks has not published studies that tested large groups of patients at their clinic, he and Levy point to a list of studies dating back decades that have linked fMRI with pain detection.
In 2009, Marks was the lead author of a paper in The Internet Journal of Pain, Symptom Control and Palliative Care that used fMRI to document pain in a 50-year-old patient with chronic neck issues. It concluded that “neuroimaging can play a useful confirmatory role in documenting the presence or absence of the sensation of pain in patients complaining of a pain syndrome.”
Though critics say that single case studies don’t equate with studies of larger groups with controls, Marks says that the body of pain-imaging research validates his work on individuals. And defense attorneys are taking it seriously. MMT has provided pain imaging reports for about a dozen plaintiffs so far, and all the cases have ended in settlements.
“We’re really at the cusp of where this is going to become standard,” says MMT’s attorney, Carlton Chen. “And as we demonstrate the reliability and standards of these tests, that they’ve been embraced by the scientific community, it is going to meet the Frye and the Daubert criteria.”
The Daubert criteria Chen refers to is a federal standard (adopted by some states) that requires judges to serve as gatekeepers to determine whether expert testimony is based on valid science, whereas Frye relies on the general acceptance of the science by the relevant scientific community.
NOT READY FOR COURT … YET
In the years since Koch’s case, researchers say, they’re even closer to reliably documenting pain through brain images. Mackey at Stanford has done studies using fMRI to detect brain activity in people who were subjected to varying degrees of heat on their forearms.
In 2010, Mackey had eight volunteers lie in an fMRI scanner while subjecting them to a heat probe, and he used an algorithm machine to identify patterns of brain activity when the heat was high or low. He then got 16 more people to lie in the scanner who were stimulated with either high or low heat, and the images were run through the algorithm, which was able to determine whether someone was experiencing pain with 80 percent accuracy.
But he cautioned that the findings were preliminary, and that the experiment was with a small group of participants only in a controlled laboratory setting.
In 2013, neuroscientist Tor Wager at the University of Colorado at Boulder led a study in which volunteers were placed in an fMRI scanner while they touched a hot plate. Wager and his team would turn the plate’s temperature up and down and record brain activity associated with the changes in temperature.
Then, using another group of volunteers subjected to the hot plate, Wager reported that they were able to predict with better than 90 percent accuracy whether the plate was warm or painfully hot by looking at the brain activity on the scan. But they were measuring acute pain under controlled laboratory settings, which is not the same as trying to measure chronic pain.
Hank Greely. Photograph by Tony Avelar.
Wager agrees with his colleagues that objective pain detection—for acute pain and chronic pain—is not ready for court, but it’s close. But also like many scientists, Wager says his work is not to serve the courts. “That wasn’t the intention,” he says. “I get the picture that people in legal settings need objective corroboration of pain.”
Wager believes that companies offering scans to document pain should be held to standards for accuracy and reliability in the same way that laboratories offering DNA evidence have been vetted by the courts. In addition, much broader studies are needed to test large populations against controls, instead of basing claims on the outcome of individual cases.
“That’s the thing we need to grapple with if these things are going to be used,” Wager says. “I think there is a lot of pressure … to use brain imagery in court now, but there are more things that need to be done.”
Chronic pain is especially difficult to identify in the brain. “The thing about chronic pain is that it comes in many variations,” Wager says. “We’re trying to figure out which brain systems track that. It’s not always clear when they say they’re in pain.”
Wager also says that emotional and physical pain appear to trigger activity in similar regions of the brain, including the anterior insula and anterior cingulate. “Romantic rejection looks similar to physical pain,” he says. “We’re working on studies to disentangle those things.”
Amanda Pustilnik, a law professor at the University of Maryland and a faculty member of Harvard University’s Center for Law, Brain & Behavior, believes legal doctrine needs to be changed to reflect that chronic pain is a neurological condition that is very real, even if you can’t prove it with a brain scan. “You can look at an X-ray of a broken leg, but we don’t have that yet for pain,” she says.
While neuroscience may not be ready to show an individual has chronic pain, Pustilnik says it has value in the legal setting. She says that experts should be allowed to testify about brain imaging—but that such testimony be limited to educating judges and jurors about the nature and causes of chronic pain—not to suggest that brain images can prove its existence or absence.
“Brain scanning technology is not a fraud-o-meter, pain-o-meter or mind-reading machine, but a tool for increasing understanding about these complex phenomena,” she says. “If what we’re really concerned about in the law is whether a person is lying about whether they have chronic pain, maybe we don’t need a pain detector but rather a lie detector. It’s an honesty question.”
Pustilnik recently joined a working group of the International Association for the Study of Pain to develop international standards for the legal uses of brain imaging. “I’m not against the use of individual brain images, but it’s still so speculative,” she says. “But the science of pain can help the legal system understand the scope of its harm.”
Hank Greely, a law professor and director of the Stanford Program in Neuroscience and Society, is optimistic that pain documentation through brain imaging is close at hand, but he says it will require passing a Frye or Daubert test for admissibility before it’s routinely accepted in the courts.
“We need to be setting up structured standards and protocols,” Greely says. “In science, we think of it as replicability.”
As these cases move to the courts, Greely says it’s essential that judges become quick studies in complex science. “Very few judges are scientists. It’s not a comfortable position for judges to be in, but they need to educate themselves in the science,” he says.
Greely believes that brain images will likely serve to buttress other clinical findings of pain, but they may not rise to the level of completely reliable. “I don’t envision a pain-o-meter,” he says. And even though companies like MMT state that their brain images work, Greely says it’s wise to be skeptical. “There needs to be transparency to how it works.”
WHAT ABOUT PHANTOM PAIN?
Professor Kolber from Brooklyn Law School raises some vital questions about the future of brain imaging for pain detection. If, indeed, brain scanning can one day objectively document pain, will that data offer a window into how the client will feel in the future? Will its duration and intensity decrease? How should it be compensated?
“You’re supposed to get damages that are associated with the actual amount of pain you’re experiencing. But we’re just so bad at doing that we have to rely on rough proxies, many times, for pain,” Kolber says.

Illustration by Sam Ward
Another key question is: Should the tort system impose penalties for those who wrongfully cause pain to others as a deterrent in the future? Kolber believes the true test of the technology will come when physicians accept it as a reliable clinical tool on which to base treatment and medication decisions. “If that were to occur, I think courts will start to accept the technology,” he says. “Billions of dollars are changing hands for pain and suffering claims, and we don’t have a lot of real good evidence about when it should and shouldn’t transfer; and it seems there would be a huge market for this if the technology gets good enough.”
University of Wyoming law professor Stephen Easton, a former trial lawyer and assistant U.S. attorney, has concerns as well. “When a case goes to trial, very often the key issue is whose testimony is believable,” he says. “We have this desire to seek a more scientific, more reliable, more precise way to define which testimony can be believed.”
There is also the concept of phantom pain to consider. “Would your brain react in the same way?” he says. “Would we compensate someone who says, ‘I have a phantom pain in my missing left foot and here’s a brain map showing it’?”
The legal system still seems to be wavering about embracing the technology. “We want more and more science. But at what point will we be comfortable to introduce the science?” Easton asks. “It’s incredibly powerful if handled well. I do think there are reasons to be cautious. What if it turns out that it’s not quite as good as we thought it was?”
The prospect of showing Carl Koch’s brain scan to a jury was apparently enough to prompt the settlement. In fact, viewing brain scans has been known to influence jurors regardless of the science behind it, and it leaves some attorneys nervous. Until the scientific evidence of pain detection is considered by higher courts, it’s still a frontier out there.
“The trouble for lawyers, jurors and judges is that we have to make a decision at a particular time,” Easton says. “My sense is that we have a ways to go before this is really available. I think this can still be very persuasive. At least the appearance of certainty is going to be very alluring, very tempting.”
This article originally appeared in the March 2016 issue of the ABA Journal with this headline: “How Badly Does It Hurt? Personal injury lawyers turn to neuroscience to back claims of chronic pain.”